The Real Cost of Wisdom Teeth Removal in Sydney: Navigating Fees, Rebates, and Savings
June 5, 2025
Wisdom Tooth Extraction and Your Jawline: Sorting Fact from Fiction
July 16, 2025
Table of Contents
ToggleMost of us grew up hearing that “crooked teeth run in the family”, yet modern evidence paints a broader picture. Studies show that breathing through the mouth, especially in childhood, can narrow the dental arches and shorten the mandible, leaving little room for the last molars to erupt. Put simply, an open mouth today may translate to an impacted wisdom tooth tomorrow. This article seeks to explore what the current science tells us and how that knowledge applies to everyday Australians weighing up wisdom teeth removal cost or wondering whether the problem can be prevented in the first place.
Why the Way We Breathe Shapes the Jaw
Healthy jaw growth rests on three simple habits: lips together, tongue to the palate, and breathing through the nose. Mouth-breathing disrupts all three. Children who rely on oral airflow typically develop longer lower faces, a steeper mandibular plane and subdued transverse growth of the maxilla, shrinking the very space third molars depend on for eruption. A recent case-control study of 70 adolescents confirmed these skeletal changes in habitual mouth-breathers compared with nasal peers. A systematic review published in 2023 echoed the link, reporting consistent findings of palatal narrowing and mandibular rotation across longitudinal cohort. Classic longitudinal work adds weight: children whose nasal obstruction was surgically relieved showed a partial ‘catch-up’ in forward mandibular growth over five years, hinting that the problem is functional rather than purely genetic.
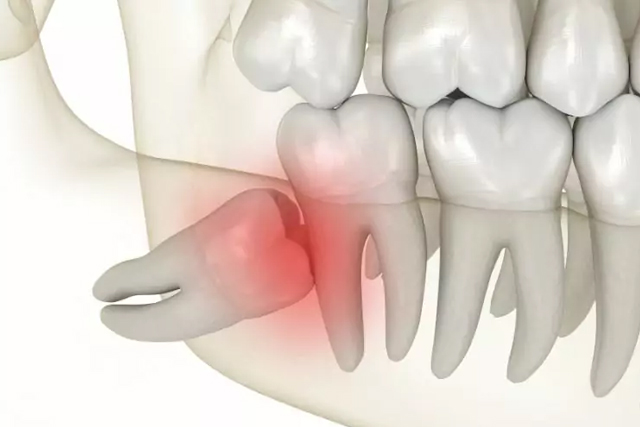
Reduced Jaw Space and Third-Molar Impaction
Third molars erupt last—usually between 17 and 25—and need roughly one extra centimetre of arch length. When the jaw is too short or the arches too narrow, the wisdom teeth Sydney stalls deep in bone. Prevalence estimates for impaction range from 17 % to almost 70 % worldwide, and mouth-breathing appears to tip the odds further by constricting oral volume. The American Academy of Oral and Maxillofacial Surgeons notes that nine in ten people harbour at least one impacted third molar, underlining how common the issue has become. Researchers at Stanford have even framed jaw shrinkage as a modern epidemic driven by soft diets and altered breathing habits, with inadequate space for wisdom teeth cited as a key downstream effect.
What the Latest Papers Say
- Systematic reviews and cohort data – Mouth-breathing leads to measurable dentofacial changes that narrow the retromolar region.
- Airway-centred dentistry – A 2022 review of third-molar management highlighted that patients with chronic airway issues often require earlier removal because their molars are more frequently mal-positioned.
- Public-health perspective – Scholars describe a “jaw epidemic” where impaction, sleep-disordered breathing and malocclusion co-exist; they argue that feeding practices and early airway care could reverse the trend.
- Surgical outcomes – Australian hospital data show that third-molar surgery constitutes a sizeable share of day-only admissions, yet complication rates remain low when evidence-based protocols are followed.
- Functional knock-on effects – Impacted molars can inflame pericoronal tissues and in rare cases contribute to airway swelling, aggravating sleep-apnoea symptoms in susceptible adults.
Practical Advice for Patients and Parents

Early Years
- Check the airway, not just the bite. Chronic snoring, allergic rhinitis or enlarged adenoids merit an ENT assessment; addressing obstruction restores nasal breathing and supports normal jaw growth.
- Encourage hard foods and lip seal. Chewing tougher textures and gentle myofunctional exercises promote forward tongue posture, widening the dental arches naturally.
Teens and Young Adults
- Regular panoramic X-rays. Radiographs taken at 16–18 reveal root development and space; clinicians can predict whether impaction is likely.
- Orthodontic expansion where indicated. Skeletal expanders can create space for the third molars if growth remains.
Adults
If symptoms emerge—swelling, pericoronitis, cystic change—extraction is generally safer than watch-and-wait. International guidelines summarise pathological thresholds and risk–benefit considerations, while recent pathology studies remind us that long-standing impactions can jeopardise the second molar and even the mandibular nerve.
Choosing a Dentist

Evidence-based management stresses practitioner volume and clear indications. A Sydney cohort study found postoperative infection rates of barely 1 % in a high-throughput university clinic. Ask how many third-molar surgeries your dentist performs each month, whether 3-D imaging is used for nerve mapping, and how pain will be controlled. Clinics that focus solely on third molars can often offer more affordable wisdom teeth removal Sydney packages because of streamlined workflows.
Key Take-Home Points
- Mouth-breathing alters jaw growth, shrinking the space third molars need to erupt.
- Longitudinal and cross-sectional research supports a functional link between airway obstruction and impaction risk.
- Australia mirrors the global picture, with most adults having at least one impacted tooth and many opting for wisdom teeth removal near me before problems arise.
- Early airway care, orthodontic monitoring and, when necessary, timely wisdom teeth removal Sydney minimise complications.
By recognising the breathing–jaw connection, dentists and patients alike can move beyond the notion that impacted wisdom teeth removal price are merely “bad luck”. Proactive airway management and evidence-based surgical care offer a clearer path—literally and figuratively—to a healthy bite and unobstructed breath.
Frequently Asked Questions
1. Does mouth-breathing really make an impacted wisdom tooth more likely?
Persistent mouth-breathing changes jaw growth by narrowing the palate and lengthening the lower face, reducing the space a third molar needs to erupt. Research in Japanese adolescents also links oral airflow to weaker tongue pressure and poorer chewing, factors tied to impacted molars. Large cohort studies confirm the trend across mixed ethnic groups.
2. When should I book a wisdom-tooth assessment, and what scans will I need?
Most Australian dentists recommend a panoramic OPG at 16–18 because root formation is visible yet removal, if required, remains technically simpler. Cone-beam CT is added when roots sit close to the inferior alveolar nerve, giving three-dimensional detail with lower radiation than medical CT. Regular reviews every two years track change.
3. What happens if I leave an impacted wisdom tooth untreated?
Untreated impaction can trigger recurrent pericoronitis, decay of the second molar, cysts and, on rare occasions, jaw tumours. Pain episodes often escalate over time and may complicate travel or exams. Mayo Clinic data note that late surgery after age 25 carries longer healing and slightly higher nerve-injury rates.