
Wisdom Teeth Removal Cost Breakdown: Consultation, X-Rays, Surgery & Hospital Fees
December 15, 2025
How to Prevent Dry Socket: 7 Essential Tips After Wisdom Teeth Removal
February 16, 2026
Table of Contents
ToggleMost people don’t notice their third molars until something feels “off” at the very back of the mouth. If you suspect your wisdom teeth coming in, it helps to know what’s typical, what’s not, and when a quick dental check can save you a week of nagging pain.
Wisdom teeth usually appear later than the rest of your adult teeth. They can come through cleanly, or they can get stuck partway under the gum, sit on an angle, or press into the tooth in front. That’s when symptoms tend to ramp up. An exam and an X-ray are often the only reliable way to confirm what’s happening behind that last molar.
Wisdom teeth symptoms you might notice first
1. Soreness at the back of the jaw
A dull ache behind the second molars is one of the earliest signs. It might flare when you chew, yawn, or clench your jaw. Mild discomfort can settle, especially if the tooth is erupting normally. Persistent pain that keeps returning is a cue to book in.
2. Swollen or tender gum behind the last molar
When the gum is stretched by an erupting tooth, it can look puffy and feel tender. If food and plaque collect there, the tissue can become red and inflamed. Keeping the area clean is harder than it sounds because it’s awkward to reach, which is exactly why irritation can linger.
3. A “flap” of gum that catches food
Partially erupted wisdom teeth sometimes sit under a small fold of gum. Food can pack underneath and bacteria can multiply. This pattern often leads to inflammation around a partly emerged tooth, a condition commonly called pericoronitis.
4. Bad taste or bad breath that doesn’t match your usual routine
If you’re brushing well but still getting a stale taste or persistent bad breath, trapped debris around a back tooth is a common culprit. Infection around wisdom teeth can also cause pus or discharge, which can create that unpleasant taste.
5. Jaw stiffness or trouble opening wide
A sore jaw joint isn’t always the problem. Inflammation around the back molars can irritate the muscles that help you open and close your mouth. If opening wide becomes difficult, or chewing starts to feel restricted, it’s worth getting checked sooner rather than later.
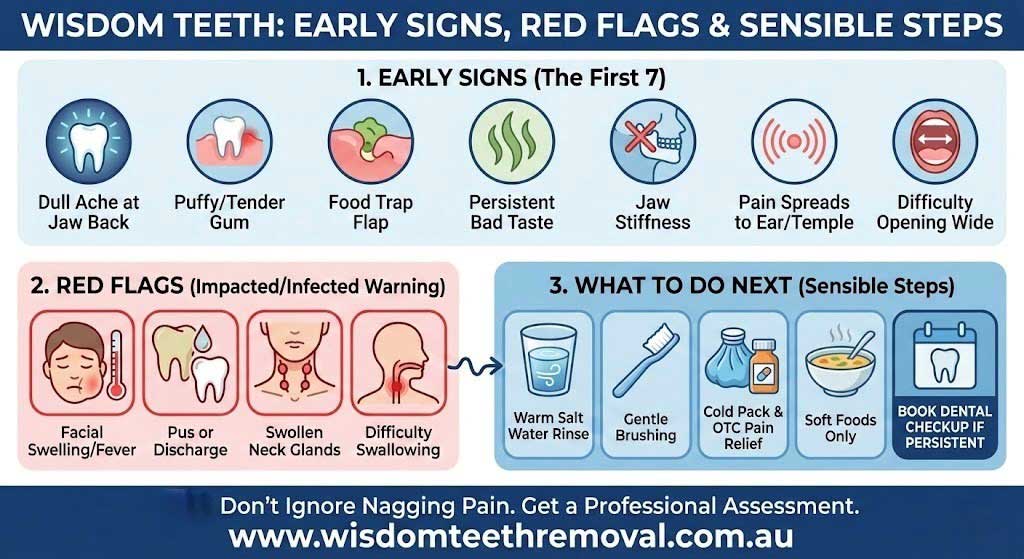
When impacted wisdom tooth symptoms point to something more than “normal eruption”
6. Pain that spreads to the ear, temple, or throat
Wisdom tooth pain can refer to nearby areas. People often describe it as earache on one side, a headache that sits near the temple, or a sore throat feeling without a cold. Spread-out pain is one reason wisdom teeth are easy to misread as “just stress” or “I slept funny”. If the discomfort keeps circling back, the tooth position needs a proper look.
7. Clear signs of infection or escalating swelling
This is the line you shouldn’t ignore. Red, inflamed gum, facial swelling, pus, fever, swollen glands under the jaw, and difficulty swallowing can occur when infection sets in around a wisdom tooth. These symptoms call for prompt dental care because infections in the mouth can worsen quickly.
What To Do Next: Sensible Steps that Actually Help
Start with the basics, even if you plan to see a dentist.
- Rinse gently with warm salt water (not boiling hot) to soothe irritated gum tissue and wash away debris.
- Brush as normally as you can, including the back area, but don’t gouge sore gums with hard scrubbing.
- For pain, follow the directions on over-the-counter medicines and avoid doubling up on products with the same active ingredient.
- A cold pack against the jaw can reduce swelling for short periods. If chewing makes things worse, stick to softer foods for a day or two and avoid small, seedy foods that lodge in gum pockets.
- Then book an assessment if symptoms last more than a couple of days, keep recurring, or interfere with sleep. Persistent toothache is a good reason to see a dentist, and an X-ray helps show whether the tooth is impacted or erupting normally.
If you’re looking for care options in Sydney, some clinics focus on surgical assessment and removal, including services such as wisdom teeth removal, which may suit people who want a dedicated pathway from consult to procedure. Get in touch with The Wisdom Teeth Professionals if you have any questions.

Frequently Asked Questions
1. How can I tell if my wisdom teeth are coming in?
Early signs tend to cluster at the back of the mouth: tenderness behind the last molars, swollen gum, discomfort when chewing, or a new spot that traps food. That said, similar symptoms can also come from gum disease, decay, or a cracked tooth. If the pain persists or keeps returning, a dentist can examine the area and confirm tooth position with an X-ray.
2. What helps wisdom tooth pain fast?
Fast relief usually comes from a mix of gentle salt-water rinses, careful brushing around the area, cold packs for swelling, and appropriate over-the-counter pain relief used as directed. Avoid poking at sore gum tissue and skip very hot, spicy, or crunchy foods for a short time. If pain is severe, worsening, or affecting sleep, treat that as a prompt to book an appointment rather than “pushing through”.
3. How do I know if my wisdom tooth is infected?
Warning signs include red, inflamed gum near the wisdom tooth, facial swelling, pus or discharge, fever, swollen glands under the jaw, bad breath, and difficulty opening your mouth or swallowing. If you notice these, don’t wait it out. Dental infections generally need professional treatment to stop them spreading and to address the cause.
4. Do all wisdom teeth need to be removed?
No. Some people have enough space for wisdom teeth to erupt and stay clean. Others have teeth that are impacted or hard to access, which raises the risk of decay or gum problems. Dentists often recommend removal when wisdom teeth cause pain, damage nearby teeth, or lead to repeated infections, while symptom-free teeth may be monitored depending on their position and risk.
5. How long is recovery after wisdom teeth removal?
Recovery varies with the difficulty of the extraction and your general health. It’s common to have some pain, swelling, and mild bleeding initially, and jaw stiffness can occur for a short period. Your dentist or oral surgeon will give aftercare instructions tailored to your case, including how to manage swelling and keep the area clean. If swelling gets worse after a few days, or you develop fever or increasing pain, contact the clinic.



